Blogs.
Heroes Among Us: How Pager’s Clinical Team Supported a Client During a Natural Disaster
by Giuseppe Diomede
When mid-September 2022 rolled around, it was certain that the weather event brewing in the Caribbean would be a powerful one should it ever make landfall. And although there was hope that the front would mercifully dissipate into a tropical storm, that was far from a guarantee. As news outlets tracked its path around-the-clock, the storm only seemed to grow more stubborn, and the reality of a natural disaster soon arriving in North America as a hurricane became inevitable. The island of Puerto Rico, still recovering from the historic Hurricane Maria in 2017, was once again bracing for impact.
Hurricane Fiona finally made landfall on Puerto Rico on September 18th, almost five years to the day after Hurricane Maria. Along with it came catastrophic flooding, landslides, collapsed bridges, and an island-wide power outage, while access to drinking water, food, and medicine became more perilous by the moment. Given the extreme circumstances and the total power outage, it would have been reasonable to expect that commerce or service - of any kind - in Puerto Rico would be non-existent for the foreseeable future.
So, it is in this context that we can only begin to understand just how heroic the efforts of Pager’s Clinical Team Call Center in Puerto Rico were.
If there is any time that virtual care and telehealth services become absolutely critical, it is certainly during a natural disaster. Understanding the urgency of the moment, Pager’s Clinical Team and Call Center in Puerto Rico sprang to action and enacted emergency protocols to remain operational. Once they discovered that cell phone towers were still functioning, Pager nurses and leadership pivoted to hotspotting and generators, circumventing inoperable WiFi and power outages to connect to the necessary triage platforms.
Some nurses located in more highly-impacted areas immediately fled to work in the safety of relatives’ homes, often several hours away. Some worked from their cars due to flooding and power outages in their homes. Any secure location with cell service was viewed as a potential workstation. And while these new arrangements were coming together, two stateside nurses along with one nurse with solar power in Puerto Rico picked up the slack by working longer hours to give their teammates’ in Puerto Rico time to get back up and running.
The Puerto Rico Call Center Manager, Joyce Green, is thrilled with the way that it all worked out. “We felt a responsibility to keep working because we knew that people would need us. And that’s what we did. I’m so proud of the way the team came together. It was business as usual for patients, and they would not have known that anything was different on our end.”
The commitment to the task at hand and the teamwork and professionalism displayed by our Call Center in Puerto Rico made for one of the prouder moments in the history of Pager.
“You become a nurse because you want to help people. Because you care about their well-being. So, the courage our nurses displayed in those difficult moments didn’t come as a surprise to me. That’s just who they are,” Nurse Supervisor Christopher Soto beamed. “I know that our nurses have that in them.”
For as humble as the Puerto Rican Clinical Team and Call Center may be, it’s worth noting that they maintained an astonishing 100% uptime, even through the weeks after the storm, when some nurses continued to work without power in their own homes. Not a moment went by where the Call Center wasn’t accessible to members seeking care in Puerto Rico because of the resolve displayed by our nurses and staff in those dire moments.
Their willpower to maintain a high level of service was recognized with gratitude by our partner in Puerto Rico. “We are grateful to Pager who has been step-by-step with us, and for their solidarity in the face of Hurricane Fiona. Their hard work, support, and donation will allow us to continue helping our community in this emergency."
Ultimately, where Hurricane Fiona brought destruction, Pager’s dedicated clinical team saw an opportunity to flip the script and turn a story of wreckage and ruin into one of relentless resolve.
5 Metrics that Prove Pager’s Find Care Solution is Best-In-Class
Find Care is all about getting members the right care, in the right place, at the right time. We do this through next gen clinical triage, care navigation, and care advocacy. These five metrics show why our solution is at the very top of the industry.
$210 savings per clinical encounter¹. Find Care saves your members the hassle of an in-person visit, the ER or Urgent Care, while saving you — the payer — money. Win-win. Which leads us to…
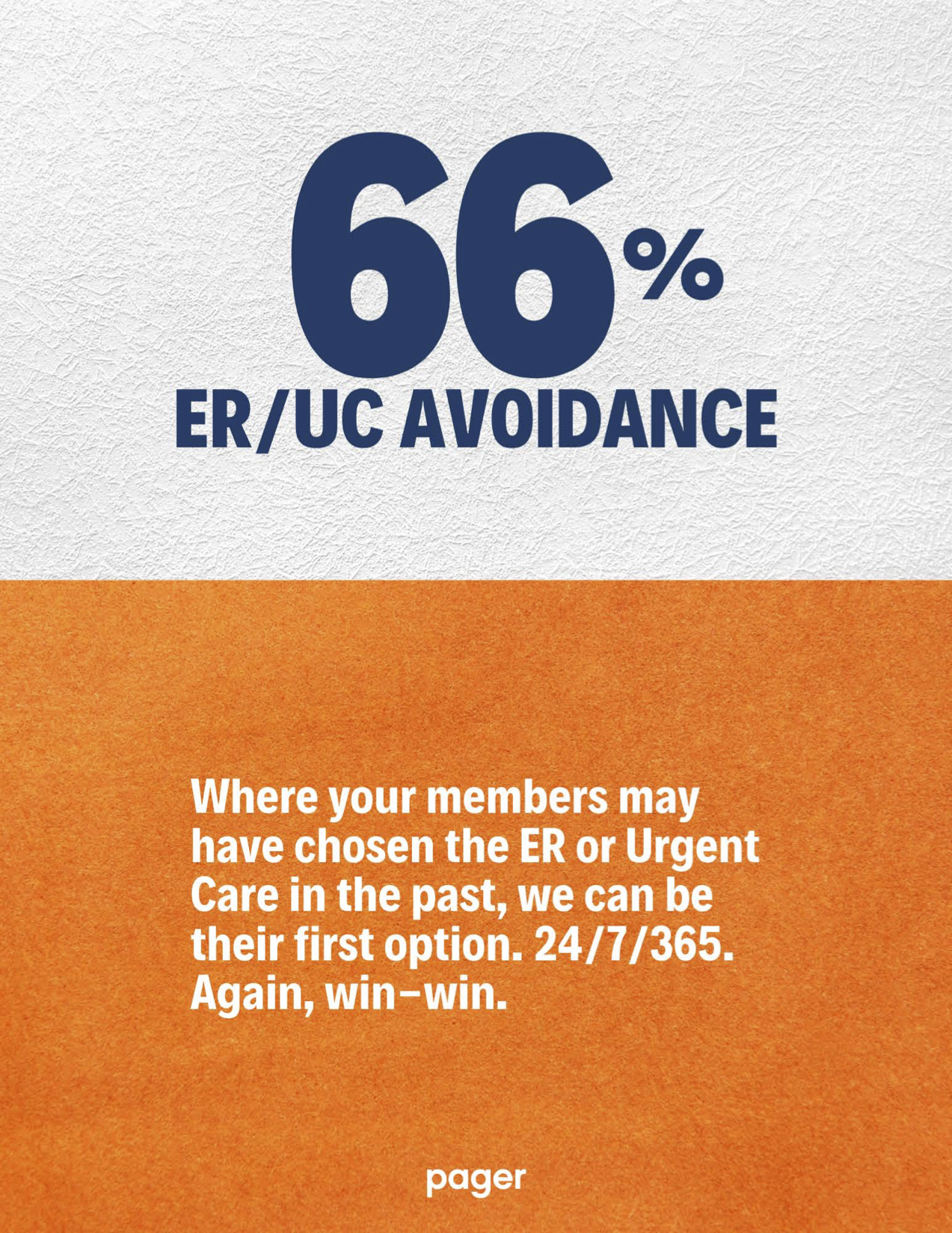
66% ER and Urgent Care avoidance. Members have traditionally looked to these two brick-and-mortar options when they’re feeling unsure or overwhelmed about a health issue. Pager’s Find Care solution curbs unnecessary visits by solving 66% of all virtual encounters outside of these brick-and-mortar locations. Again, win-win.
Time-to-first touch in 30 seconds or less. When your members reach out to us for care, we don’t leave them waiting. They’ll thank you for making their care experience easier and more efficient and helping them get back to living their lives with peace of mind.
A customer satisfaction (CSAT) score of 98%. CSAT measures happiness with a product, service, or customer support interaction. Health insurers and hospitals score an average of 73 and 76 respectively. With Pager, you get a 98%, showcasing our dedication to exceptional member experience, which boosts your member retention and bottom line.
NPS score of 88+. NPS is considered the ‘holy grail’ for understanding customer satisfaction and loyalty. For context, scores above 50 are considered 'Excellent', and 38 is the average in the healthcare industry. A score of 88+ is rare, but that’s where Pager ranks. And because we’re white-labeled, the NPS is attributed back to the health plan, leaving members extremely loyal.
Do you want a closer look at how Pager is able to offer your members a seamless healthcare experience? Head to pager.com/demo, and let us show you how we do it.
¹ Numbers from an actuary study conducted in 2020 from a large health plan in their commercial line of business.
Case Study: After Care Drives Member Engagement and Fills Care Gaps
As virtual healthcare evolves, we see lower costs for the insurer and their members, as unnecessary visits to the ER, Urgent Care and doctors’ offices have been slashed. Patients may have reduced co-pays and can receive care for common issues wherever they are at the moment they need it. The benefits are obvious.
But for as transformative, convenient, and cost-effective as virtual healthcare can be, it can leave some care gaps that don’t necessarily exist in brick-and-mortar healthcare:
• Interactions with care providers can be more transactional than personal.
• Next steps in care may not always be clear to the patient.
• Care can feel issue-specific and not take into account the bigger picture of the member’s health.
With these challenges in mind, there is one question that drives the work we do at Pager:
How do we ensure the member has an authentic, human connection with their care providers while also filling the gaps that traditional virtual care creates?
One way we answer this question is with what we call Pager After Care.
The Pager After Care solution allows us to check in on the wellbeing of patients several days after their initial visit with a Pager care team member to address any gaps and barriers patients are experiencing. For example, our nurses will schedule a follow-up appointment with the patient at the end of their initial visit with a doctor, and during the follow-up itself, the nurse reviews the patient’s progress and response to their care plan, adherence to medication, or preventative steps they’ve taken to alleviate recurrence of the issue.
We see the After Care solution as an opportunity to form a personal relationship with the member, whereby the member inherently feels cared for by real people aided by technology and not the other way around.
Joe Martinez, Vice President of Virtual Care at Pager, sees After Care as a critical element to developing better holistic care. “After Care gives us an opportunity to provide more robust care. Maybe it's another nurse triage, helping patients find a doctor, scheduling an appointment for them, or connecting them with the appropriate resources they need.”
“We're seeing more patients utilize virtual care than in years past. Patients are thankful our care team members are routinely checking in on them to make sure they are doing better- a practice that is unique in virtual healthcare. And when they feel better, they have more energy to talk to us about other concerns that we can help address, and therefore be proactive about how we manage their care holistically,” says Pager’s Nurse Manager, Matthew Morin.
While we continue to implement new and improved After Care protocols on a rolling basis, the data shows the value of the program to health plan members:
• The member response rate to the Pager After Care Program is 68%, showcasing how many members need - and benefit from - clinical follow-ups.
• 73% of members reported improvements to symptoms after speaking with the Pager nursing team.
• 72% of patients who did not previously have a Primary Care Physician were connected to one in-network.
• 45% of members were provided additional education on diet/exercise, injury prevention, and family planning.
• 78% were prescribed new medications post navigation, and of these, 45% required additional education on medication, information on side-effects, and details on claims and benefits, to name a few.
Joe Martinez adds, “After Care gives us meaningful health data that provides us an opportunity to build a partnership with patients, since we have a moment to talk to them and inquire about what's important to them.”
As the data we harness continues to get more sophisticated, we’ll be able to help patients with long-term and specialty care. There will be opportunity to leverage our established relationships with them to see the big picture of their overall health, and because of that, patients will be cared for in an even more specific and personal way.
Matthew Morin is excited about the future of Pager After Care. “We see ourselves building in more preventative screenings and adding questions to address additional needs. As our processes evolve along with our systems, we’ll find new ways to target individuals so that we can provide more specific questions that relate to them and their health journey.”
The Four Pillars of Pager’s Powerful Enterprise 360 Solution
Pager Enterprise 360, or E360, is our SaaS-based solution that addresses three common challenges in digital health care: engagement, fragmentation and burnout.
Most digital health care is driven by point solutions, where one-size-fits-all.
With E360, we facilitate real engagement by giving care providers the ability to be more specific and more personal. And it all happens on a single platform, eliminating the fragmentation and clutter of most digital care experiences that rely on multiple apps. Most importantly, because E360 allows providers to use A.I. to enhance their care support, they can provide member solutions more quickly and accurately, curbing the burnout that can occur when the care ecosystem is overwhelmed.
Pager’s Enterprise 360 solution can be broken down into four digestible pillars, all showcasing the benefit and state-of-the-art experience you receive when you deploy this platform at your health plan.
Seamless Collaboration: Think Slack for Healthcare. Communication, workflow and synergies across care teams. An experience that allows for more than 30+ roles at a time to be working within a single interface, which enhances the quality of member care and service.
Plug-In Architecture: Turnkey integrations across all of your current vendors and platforms. This “plug-and-play” architecture allows for a new level of efficiency, scale and workflow management. E360 provides flexibility and allows for system and app integration so that you can use the technological solutions that already exist in your ecosystem… all within a single place.
Agent ‘Superpowers’: Clinical and non-clinical agents are equipped with the tools that provide efficiency so they can focus their time on patient care and quality. Some of the tools provided at their fingertips include:
Scalability: E360 is built to grow with you over the lifetime of your growing membership base.
• 4:1 chat concurrency, enabling agents the ability to handle more patient volume.
• 30+ roles created for any clinical or service agent on the platform.
• 7,000 agents (and counting!) currently deliver care to patients on the platform.
• AI-driven Actionable Insights (follow-up reminders, members with care gaps, etc.)
• Access to Integrated Patient Data from Other Internal Systems
• Warm Hand-offs Between Agent Roles
• Schmitt-Thompson Protocol Triage Guidance
• Bot-led Questionnaire & Symptom Checker
• Canned Responses for Timely Communication
• Agent-to-Agent Chat
• Omnichannel Communication for the Member: Chat, Voice & Video
In the digital health care landscape, E360 elevates your current set of offerings in a way that is unique, forward-looking and perhaps most importantly, scalable. It leverages technology to empower care providers to be the experts they are while making the customer experience simple, timely and clutter-free.
Let us show you how we do it by going to pager.com/demo.
End-user story.
This content was originally used on LinkedIn as a carousel but is re-purposed for other formats as necessary. E360 is a powerful one-of-a-kind product in the digital health care market.
Product overview.
Product highlights.
Product preview.
Miscellaneous collateral.
These graphics are all used for various purposes- as sales collateral, social media posts and presentations as needed.